Those of you who know me well are probably tired of hearing it's been a tough year, blah, blah, blah. It has been. My group at BURRIS and I have gone through a transformation for the business that has at once been optimistically conceived and realistically implemented. In other words, we work hard to be what we think we need to be to be successful, but there have been times when we've actually been what we HAD to be in order to make payroll.
Anyway, no more on that. I promise. I'll save it for the history book ... or for the eulogies someone else can deliver.
When you're going through the daily slog, however, sometimes trying just to get it to the next day, the last thing you need is to get bogged down by something you count on working smoothly. Yesterday was one of those days when - well, geez, I just can't believe what happened.
Apparently it began last week. Our own Lyn "I do it all" Rollins was on vacation, apparently doing what we all do when we're on vacation: she was in the drive-thru line at her local pharmacy picking up a prescription. The attendant on the other side of the metal drawer informed her that her - our - insurance had been cancelled, and Lyn would have to supplement with more than her share of the co-pay.
Now, fortunately, Lyn is also the person responsible in our little company for the relationship with UHC, United Healthcare, our healthcare insurance provider. So after getting over the shock of learning we've been cancelled, she pulls her car to the side and dials up her contact to ask what's up.
A bit more background...
Faced with a 20%+ increase in premiums and the de rigueur reduction in services, we cobbled together a different employee health insurance plan this past Fall. The new program (I don't recall the reason, but it probably didn't make sense then either) could not be enabled 'til the beginning of the calendar year, so what we had to do was offer a kind of amalgam of the old and new from October through December, then transition to the new program on January 1. (Stay with me a second; this really is relevant.)
So for three months, Lyn (who also, by the way, pays the bills) would send a check to UHC, and they were to apply one portion of the payment to one program, another to the, uh, other program. Sounds confusing, but this is what UHC required.
Well, apparently, what UHC's accounting department was doing was applying one portion, but not the other. So come premium-due-day recently, with an eye for folderol and armed with a bureaucratic, "this is how we do it" policy, some QWERTY-striker at UHC double-lined us from the rolls of active premium payers, incorrectly considered us policy non-paying deadbeats, and - this is the kicker - cancelled one of the key parts of our "amalgam" coverage.
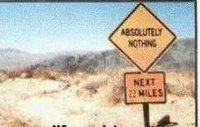
No call, no registered letter, no email, no visit ... nothing. Poof! Cancelled.
Doomsday scenarios are everywhere in this kind of thing, but, fortunately, the worst thing that happened (we think) is that Lyn was denied co-pay at the pharmacy.
But there have been plenty of the "can you believe?" questions in the last few hours.
For instance, can you believe that UHC still hasn't straightened out their accounting mess? Can you believe we had to wire ("Wire!") a partial payment yesterday to cover the account? (They couldn't just move the overpayment for the one they credited to the one they didn't.) Can you believe that it takes 48 hours before our prescriptions policy can kick back in? And can you believe that no one with whom Lyn has spoken from UHC can explain why this happened, why they didn't contact us BEFORE cancelling our policy? Much less apologized for the inconvenience.
We all have (and continue to) read about the problems, the crisis in healthcare this country faces. It's just too much for me when I compound that with the combination of hubris and ineptitude that we have faced on more than one occasion with United Healthcare.
There's no way these people could survive if they had to perform the way a normal business does.
 The last of my holiday reading was Gabriel Garcia Marquez' latest little book, the beautiful "Memories of My Melancholy Whores."
The last of my holiday reading was Gabriel Garcia Marquez' latest little book, the beautiful "Memories of My Melancholy Whores."